The COVID-19 pandemic has taken its toll on the mental health of people all over the country, including those who are commercially insured.
Our 2022 Workforce Health Index shows that, in 2021, one in four individuals self-reported feeling down, depressed, or hopeless several days over a two-week span, a 21% increase from 2019. In 2020, almost half of all telehealth visits addressed behavioral health needs, which is especially significant considering telehealth utilization grew by nearly 30X from 2019 to 2020. And in 2021, behavioral health grew to an even larger share of total virtual visits, reaching almost 60%.
However, while the pandemic certainly had a severe impact on mental health—which is to be expected when you combine factors like social isolation, burnout, unexpected loss, and more—this is far from a novel issue. Behavioral health medical spend has seen double-digit growth rates annually since at least 2018.
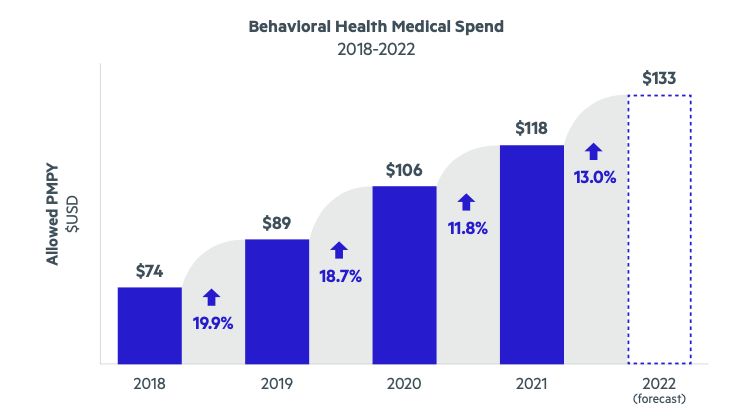
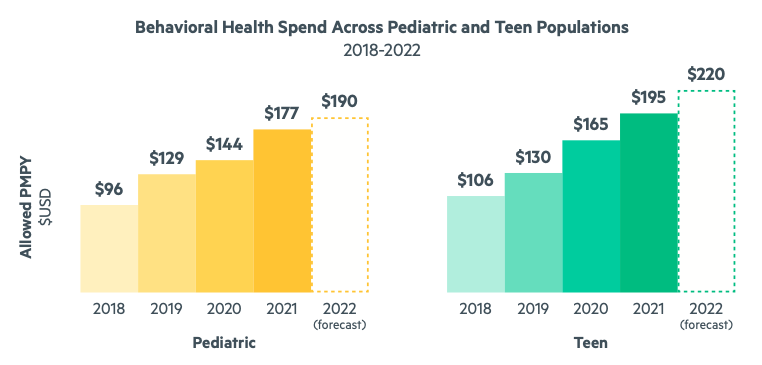
Just as alarming—if not more—is the fact that these trends are more pronounced among pediatric and teen populations. Not only is the need for behavioral and mental health support growing for younger populations, but the rate of increase and the average cost of mental health care is higher for children and teens than it is for adults. For teens, the growth in behavioral health spend was 26.9% in 2020 and 17.9% in 2021. For children, it was 11.5% in 2020 and 22.7% in 2021. Our comprehensive analyses predict that in 2022, per member per year (PMPY) behavioral health medical spend will be $190 for children and $220 for teens, compared to $133 for adults.
Fortunately, employers have taken note of this national crisis. In 2021, 78% offered some type of behavioral health program, up from 54% in 2019. This is great progress, and we commend those employers who are stepping up to better support their people. However, offering services doesn’t guarantee employees and their families will engage and truly get the care they need.
That’s where Castlight comes in.
Castlight’s Clinical Interventions Framework
Personalized recommendations are key to helping members take the next best step in their unique health journey. One way we ensure we’re surfacing the right recommendations for each member is by leveraging our Clinical Interventions Framework, an evidence-based, rigorous, and systematic approach to personalizing each member’s health journey with the goal of engaging them in high-value, clinically-validated interventions.
Whether a member is healthy or managing a chronic condition, this framework is the guiding light to how we identify and prioritize recommendations that achieve high-value clinical goals.
This proprietary framework is anchored on seven universal clinical goals we want to help every member achieve, plus a list of interventions we’re able to offer to support each goal. To choose our goals, we focused on chronic conditions and other areas of clinical need (e.g., pregnancy and preventive care) that we know are tremendous drivers of healthcare spending and offer opportunities for better outcomes.
For each condition and intervention, we completed an extensive review of evidence-based guidelines—U.S. Preventive Services Task Force, American College of Physicians, American Academy of Orthopaedic Surgeons, American College of Cardiology, The American College of Obstetricians and Gynecologists, and Choosing Wisely—to ensure our approach is up to date and aligned with the latest expert advice.
One of the seven pillars of the framework is ensuring members get behavioral health support. Our rationale for making this one of the seven clinical goals is that, in addition to the fact that taking care of one’s health extends beyond just the physical, behavioral health diagnoses can greatly increase medical spend. In addition to the Workforce Health Index findings mentioned above, we know that:
- In 2015, the total economic burden of major depressive disorder was estimated to be $211 billion per year, a 22% increase from 2005
- In 2019, 21% of U.S. adults (52.9 million people) experienced mental illness
- In 2020, 8.4% U.S. adults (21 million) had at least one major depressive episode
- Depression is a leading cause of disability worldwide
When we identify a member who needs behavioral health support of some kind, we steer them toward high-value and clinically-validated solutions (ideally covered by their employer), such as a provider or a digital behavioral health solution—like one of our mental health-focused Ecosystem partners: Total Brain, Whil, meQuilibrium, 2Morrow, Spring Health, myStrength by Teladoc Health, Vida, Daylight, and more.
Care Guides in Action
Castlight’s Care Guides, our team of clinical and benefits experts, can play a vital role in ensuring members are aware of and able to access resources, programs, and services available to them—including making sure those who need behavioral health support can get it.
Here are some examples:
- Like many others, Meg* was feeling overly stressed due to the pandemic. Because she has a history of anxiety and depression, she decided to reach out to Care Guide Pam for help. First, Pam made sure Meg had no current suicidal ideations and and that she was aware of suicide prevention resources available to her just in case. Then, she helped Meg obtain mental health support. At the time, this was quite difficult, as most high-quality providers were booked for months. But Pam was determined—she kept calling and leaving voicemails until she was successful. Today, Meg sees a therapist regularly.
- Jane* originally reached out to Care Guide Caren to learn more about a wellness email she’d received from Castlight. During that call, Caren discovered a few other issues Jane was struggling with, including navigating overwhelming sadness and grief resulting from the traumatic death of a family member. Caren collaborated with Jane’s EAP to connect her with a therapist, in addition to researching local Spanish-speaking grief support groups Jane could partake in.
- When Ed* reached out to Care Guide Dallin asking for help with substance abuse issues, Dallin got to work. He researched the different resources available to Ed (including counseling services through his EAP) and connected him with a clinical Care Guide who was able to discuss the situation from a clinical perspective. Ed was surprised and relieved that the Care Guides team helped him get help for this issue without judging him.
These are just a few examples of how Castlight’s amazing Care Guides have helped our members connect with the behavioral and mental health support they need.
*Names have been changed for confidentiality.



