Mental health concerns were prevalent before COVID-19, with one out of five U.S. adults diagnosed with a condition. Currently, over half of adults in the U.S. report that the pandemic has negatively affected their mental health. Thus, the need to address behavioral health symptoms has never been more urgent.
The good news is that there are highly effective therapies for common mental health conditions such as cognitive behavioral therapy and medication therapy. However, only just over 40% of U.S. adults with a mental health condition report receiving care. To address the most common barriers to behavioral healthcare including access, awareness, and affordability, it is critical for employers to understand: How have the mental health needs of employees and their families changed as a result of the COVID-19 pandemic?
Awareness remains a barrier
Since the pandemic started, Castlight’s users report moderate to high levels of stress (81% of survey respondents), insomnia (84%), anxiety (82%), and depression (76%). However, many employees remain unaware of the behavioral health resources provided as a part of their health benefits.
A key to raising awareness targeting not only those that have a diagnosis, but identifying those who are at-risk based on their responses to health risk assessment questions, in-app surveys, searches, and other activities.
To help people understand programs that are best for their unique needs, employers should provide easily-accessible behavioral health tools which can in turn help employees realize they may need care for a behavioral health condition. Castlight’s behavioral health solution can help employers meet these needs with customized outreach to members through email, in-app, and with Clinical Care Guides.
Engagement with behavioral health programs is strong
While people are reporting increased symptoms of behavioral health conditions, the good news is that Castlight sees strong engagement with behavioral health programs. This is true across the spectrum of resources—from 30% engagement with resilience tools, to 10% with teletherapy programs.
Care delivery is changing, and it is dramatically improving access
In the U.S., the average wait time to see a therapist is 21 days, and a shocking 60% of counties in the U.S. do not have a dedicated behavioral health practitioner. These barriers to timely access of mental healthcare are worsened by the very nature of behavioral health conditions which may reduce one’s capacity for navigating the complexities of the healthcare system.
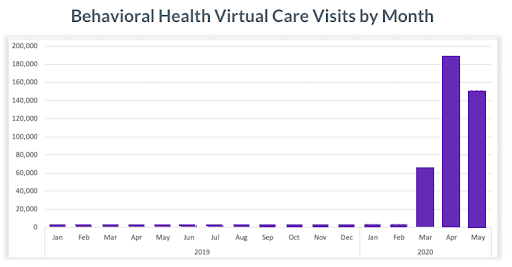
As part of the CARES Act passed in March 2020, teletherapy is a more widely available option for employees seeking mental health support. Castlight data demonstrate that members have increased telehealth visits for behavioral health by nearly 20 times since the beginning of the pandemic in the U.S., and behavioral health appointments have encompassed nearly one-third of all telehealth visits since March.
Given the national scarcity of behavioral health specialists, primary care providers have an important role in serving patients with behavioral health conditions, including those who are undiagnosed. More than 90% of all medication therapy for behavioral health conditions are prescribed by primary care providers.
This changing landscape offers a good opportunity for employers to promote existing resources at a time when people are increasingly searching for behavioral health support. Castlight Behavioral Health suggests care that members are best able to access — whether through their primary care providers, behavioral health practitioners, teletherapy, or employer-sponsored digital health programs.
Members with a behavioral health condition have broader care needs and higher costs
Over 40% of U.S. adults with a behavioral health condition cite cost as a top barrier to their ability to access care.
To address this, employers need to help employees navigate to free and low cost options in their healthcare offerings, including employee assistance programs and digitally-enabled cognitive behavioral therapy. For those with diagnosed conditions and elevated needs that require in-person care, Castlight’s integrated provider search navigates them to the highest-quality, cost-effective provider in their network.
In addition to affordable options for behavioral health resources and care, there are also broader care implications which makes the needs of individuals with a diagnosed behavioral health condition more complex, and more costly. Of Castlight members with a diagnosed condition, only 36% saw a primary care provider in the last 12 months, 11% have been hospitalized in the last 18 months, and 4% have overutilized the ER in the last year.
As a result, members with an underlying behavioral health condition spend 2x as much compared to members without a condition. Castlight helps employees and employers save on medical costs, with savings ranging from 10% ($212) for low risk users to 4.4% ($698) for high risk.
Conclusion
As Castlight Chief Medical Officer Dr. Dena Bravata explains, “Emotional wellbeing is important for everyone, but it is a different issue for everyone.” Meeting employees’ behavioral health needs requires a holistic approach that addresses awareness, access, and affordability.
At Castlight, we understand that resources to respond to the growing behavioral health crisis are more urgent than ever. As a response to the COVID-19 pandemic, in June we made our Castlight Behavioral Health offering free to all Castlight Complete customers.
From offering direct in-app resiliency programs to guiding users toward teletherapy or in-person care, employers can take advantage of existing tools to ensure their entire workforce is able to access cost-effective, quality care.