By far, one of the top drivers of healthcare costs in the United States is the management of chronic conditions — and today, almost 147 million Americans are living with at least one. The average annual medical spend for individuals with a single chronic condition is $7,000 to $19,000, but many people are living with two or more, compounding costs even further.
During the pandemic’s early days, Castlight observed steep declines in preventive care services of up to 70%, despite skyrocketing telehealth rates. Though preventive care utilization has returned to pre-pandemic levels, this doesn’t offset the overall decrease — many people still aren’t getting the care they need. This is important to note because preventive care plays a critical role in diagnosing chronic conditions and developing treatment and management plans.
On the bright side, there has been a large upsurge in the number of digital health programs, and consumers are increasingly embracing the use of these tools. Of course, this increase in program volume and utilization presents some challenges, too. Currently, the average employer offers an average of 14 different point solutions, with some providing more than 20. This is a complex administrative endeavor for benefits leaders and a barrier for employees to access and understand which programs are best suited for their individual needs.
Recently, Castlight hosted a webinar with Anoop Sangha, MD, vice president of Clinical Programs at Teladoc Health, Candace Quagliato, SPHR, lead benefits analyst at WestRock, and Heather Hagg, PhD, vice president of Analytics and Operations at Castlight Health, discussing the important role organizations can play in helping employee populations manage chronic conditions and how partnering with a health navigation platform can result in higher engagement, better clinical outcomes, and cost savings.
The Case for Digital Condition Management Programs
Though today’s healthcare system is well-equipped and prepared to manage acute care, such as a heart attack or stroke, it simply isn’t set up to adequately support those living with a chronic condition. “People spend 99.9% of their waking hours outside of the healthcare system, where they’re left to manage the condition on their own,” says Sangha.
That’s where consumer-focused digital health programs — like Livongo, which was recently acquired by Teladoc and provides solutions for diabetes, high blood pressure, weight management, and behavioral health — can help. Programs like these empower members to achieve an improved health status by removing behavior change barriers and helping each individual figure out how to best fit condition management into their daily schedule.
How Castlight Elevates Digital Condition Management
Castlight builds deep integrations with all benefits offerings — including our ecosystem of condition-specific point solutions, provider and cost transparency tools, employee assistance program information, and other wellbeing programs — and centralizes them into one single, seamless experience.
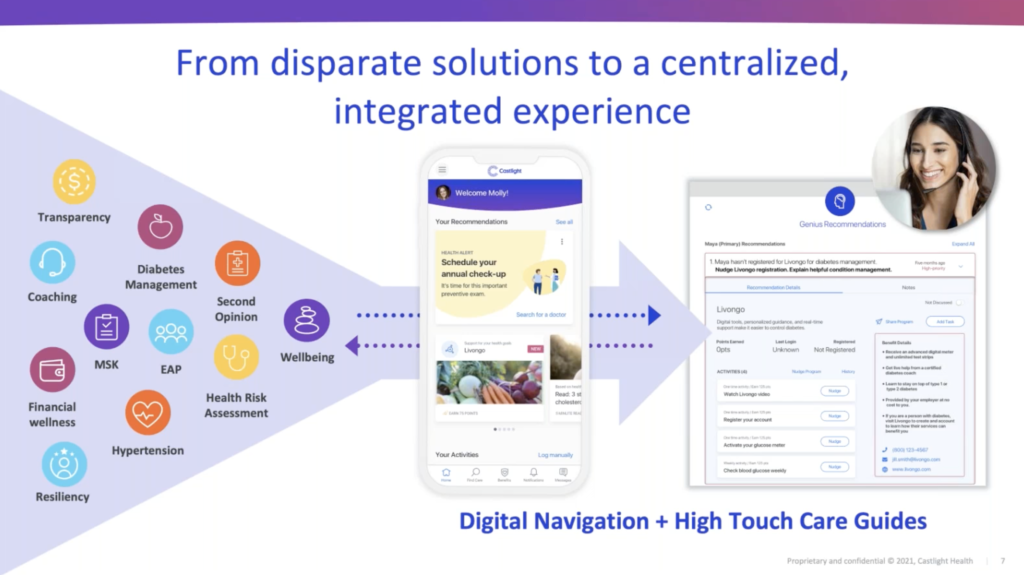
Employees can access all of their benefits digitally and seek support from Castlight Care Guides, our team of highly trained and experienced benefits and clinical experts.
In addition, by leveraging a vast and diverse set of medical, wellbeing, search, and socioeconomic data, we can group individuals into different categories. Within each one, we create subgroups so we can tailor our program recommendations to be as relevant as possible to each member, which is critical to engagement. A person who has type 2 diabetes, for example, should receive different guidance than someone who’s only at risk for diabetes.
Personalized recommendations, however, are not enough. To meet users where they are, we tailor our outreach methods based on individual preferences. While some respond better to digital notifications, others prefer chatting through the app or phone. “By leveraging different outreach methods through a connected omnichannel experience,” says Hagg, “we see higher engagement and the ability to more effectively guide people to the right programs and care.”
The Results of Partnering with a Health Navigation Platform
While our partners already drive strong engagement on their own, partnering with Castlight makes a big difference. Across our customer base, participation in diabetes, musculoskeletal (MSK), and hypertension programs increases significantly when people access them through Castlight.
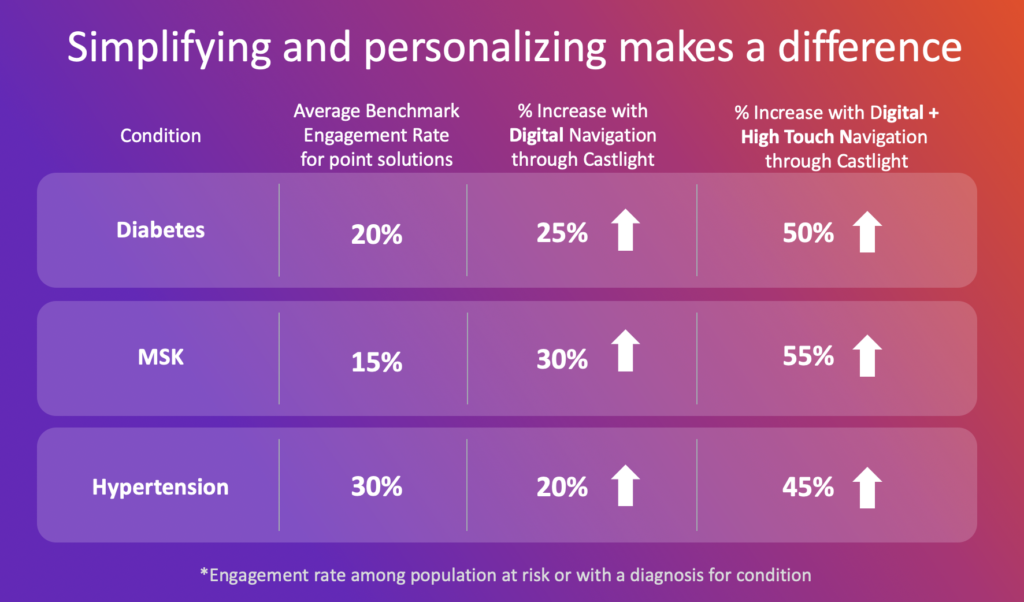
“Livongo is very excited to be partnered with Castlight,” says Sangha. “We’ve seen a tremendous impact. Castlight’s health navigation platform is helping to direct the right people to Livongo.”
Independently, Livongo yields an impressive 34% engagement rate — but with Castlight, the average engagement rate with Livongo is 43%. “Castlight is truly employing a best-in-class engagement approach for a chronic condition program,” Sangha says. “And we know that, once we can get people to engage with a program, we’ll be able to produce behavior change that ultimately translates to clinical results.”
In addition to improved health outcomes, we’ve found that when we partner with digital solutions, together we’re able to drive savings of between 50% to 60% for members who are living with top chronic conditions — members who engage with a digital health program via Castlight experience significantly fewer ER visits and inpatient admissions.
How WestRock Is Helping Employees Manage Chronic Conditions
At WestRock, a leading global packaging company with more than 320 locations in the United States and almost 60,000 members enrolled in benefits, the top chronic health condition among their population is diabetes. The company decided to tackle this problem by partnering with Livongo, which they provide to employees for free.
To roll out this new offering, WestRock employed a multi-step approach:
- Centralize: All of WestRock’s health and wellbeing benefits live in a single digital hub on the Castlight platform in order to provide a frictionless experience for employees.
- Embrace human-first promotion: The benefits team asked WestRock leaders to tell their teams about the program. Word of mouth really helped fuel uptake. “Once one person in a location enrolls and has a positive experience,” Quagliato says, “word gets out pretty quickly and other people start to enroll.”
- Personalize outreach: Leveraging claims data, biometrics results, user behavior, and other information, Castlight and Livongo enabled WestRock to identify and reach out to those who would benefit from a diabetes program.
- Incentivize engagement: Castlight, Livongo, and WestRock partnered together to choose specific micro-behaviors that will encourage user engagement, such as enrolling in the program, watching an educational video, and checking in once a week with their glucose monitor. When members complete one of the chosen activities, they can earn points in the Castlight rewards center, and those points translate into dollars.
Ultimately, 53% of WestRock employees currently living with diabetes engage with Livongo through Castlight, as do 21% of employees who are at risk for diabetes. This has led to real cost savings for the company. Overall, WestRock is saving an average of $133 per diabetic episode — and for members living specifically with type 2 diabetes, the per-episode savings is $321.
To hear more about how employers can approach chronic condition management, watch the webinar. To view all of our past webinars and register for upcoming webinars, click here.